Turning and Positioning: Vital Steps for Pressure Redistribution

Considerations for Turning and Positioning: General Guidelines
- Check Pressure Points: Ensure all pressure points are adequately offloaded by checking that pressure areas receive intended relief. In the lateral side-lying position, offload the sacrococcygeal area without placing pressure on the trochanter.
- Self-Relief Education: Teach individuals who can provide some or all their own pressure relief to reposition correctly and perform 'pressure relief lifts' or other maneuvers.
- Heel Care: Pay particular attention to the heels, which can be continuously exposed to pressure even with frequent repositioning. Refer to the guidelines on heel pressure injuries for specific recommendations.
- Ventilated Patients: For sedated and ventilated individuals, particularly neonates and infants, frequently reposition the head.
- Medical Devices: Avoid positioning the individual directly onto medical devices like tubes or drainage systems. Refer to guidelines on device-related pressure injuries for relevant recommendations.
Turning and Positioning for Individuals with Pressure Injuries
|
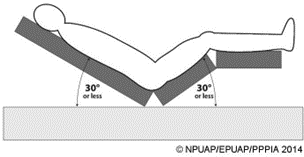
1. Existing Pressure Injuries: Avoid positioning the individual on bony prominences with existing non-blanchable erythema. 2. Preferred Positions: Use the 30° side-lying position instead of the 90° side-lying position. Encourage individuals who can reposition themselves to sleep in a 20° to 30° side-lying position or flat in bed if not contraindicated. 3. Head of Bed Elevation: To minimize pressure and shear, it's recommended to keep the head of the bed as flat as possible. Avoid elevating it beyond 30°, especially for critically ill individuals at high risk of pressure injuries, as higher elevations increase interface pressure at the trochanter and sacrum.
4. Shear Prevention: Prevent sliding down in the bed by flexing the knees and using pillows under the arms. This helps avoid shear forces and weight-bearing on the sacrum and/or coccyx. 5. Eating Positions: For individuals with a sacral and/or coccygeal pressure injury, sitting erect on the side of the bed while eating may be a better option. Ensure integrated bed systems that transform into a chair position do not place direct pressure on the injury. |
 |
- Assessment: Before repositioning, assess the individual's current position and any pressure points.
- Lift, Don’t Drag: When repositioning, lift the individual to avoid dragging, which can cause shear forces and increase the risk of skin damage.
- Optimal Offloading: Position the individual to offload pressure from bony prominences and distribute pressure evenly.
- Use Supportive Devices: Utilize pillows, wedges, and other supportive devices to maintain the new position and offload pressure areas.
- Regular Monitoring: Frequently check the individual's skin condition and the effectiveness of the pressure redistribution. Adjust the frequency and method of repositioning as needed based on the individual's response.