Clinical Practice Guideline for Optima Prone
Risk factors and development of pressure injuries
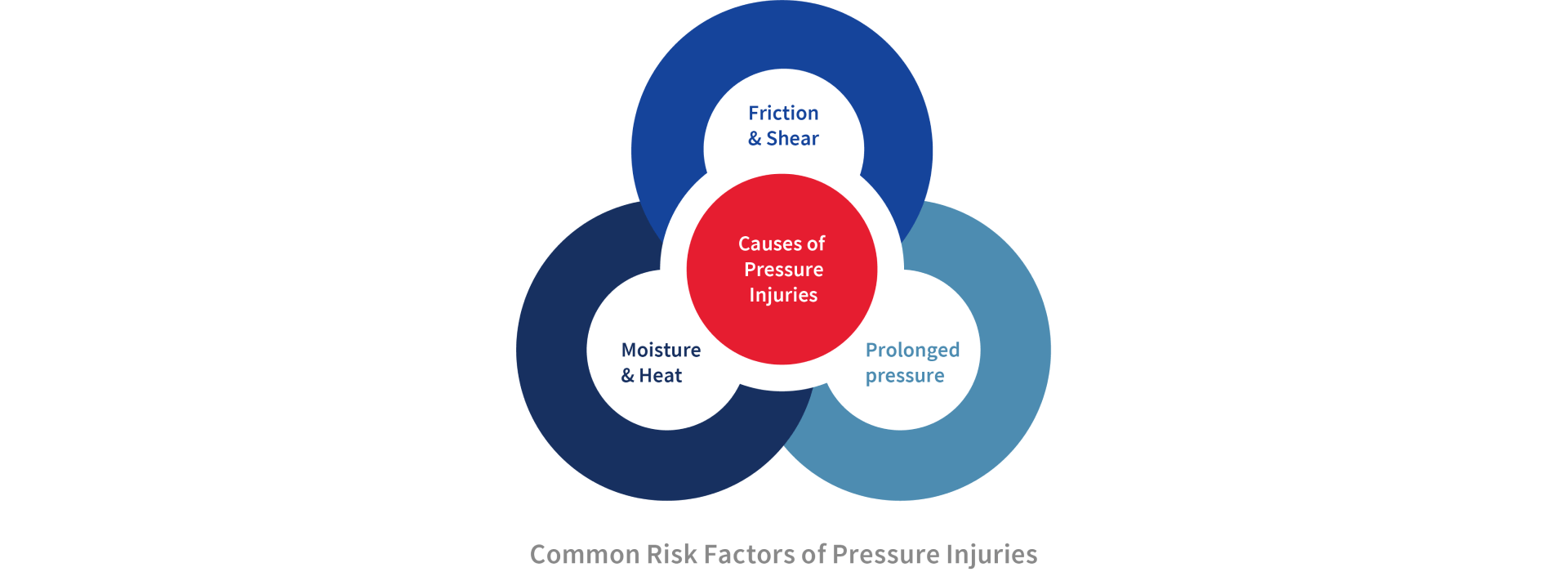
Pressure Injuries commonly occur as a result of tissue being exposed to prolonged pressure or pressure associated with friction & shear, or the weaker tissue caused by moisture.1
Pressure injuries are categorized into 6 stages: Stage I with a non-blanchable erythema of intact skin; Stage II with a partial-thickness skin loss with exposed dermis; Stage III with a full-thickness skin loss; Stage IV with a full-thickness skin and tissue loss; Unstageable pressure injury is defined as obscured full thickness skin and tissue loss; And last, Deep tissue pressure injury is the persistent non-blanchable deep red, maroon or purple discoloration of the skin.2
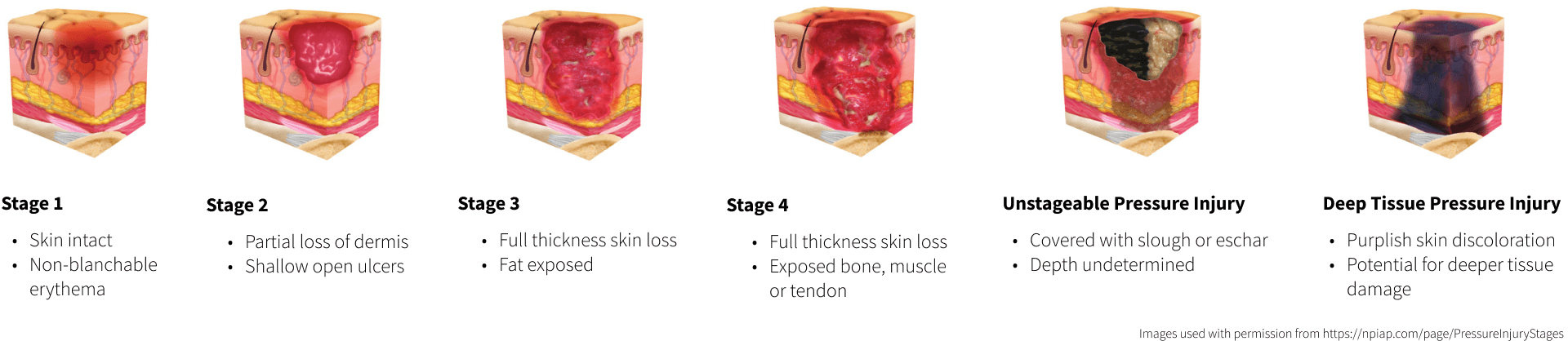
Images used with permission from https://npiap.com/page/PressureInjuryStages
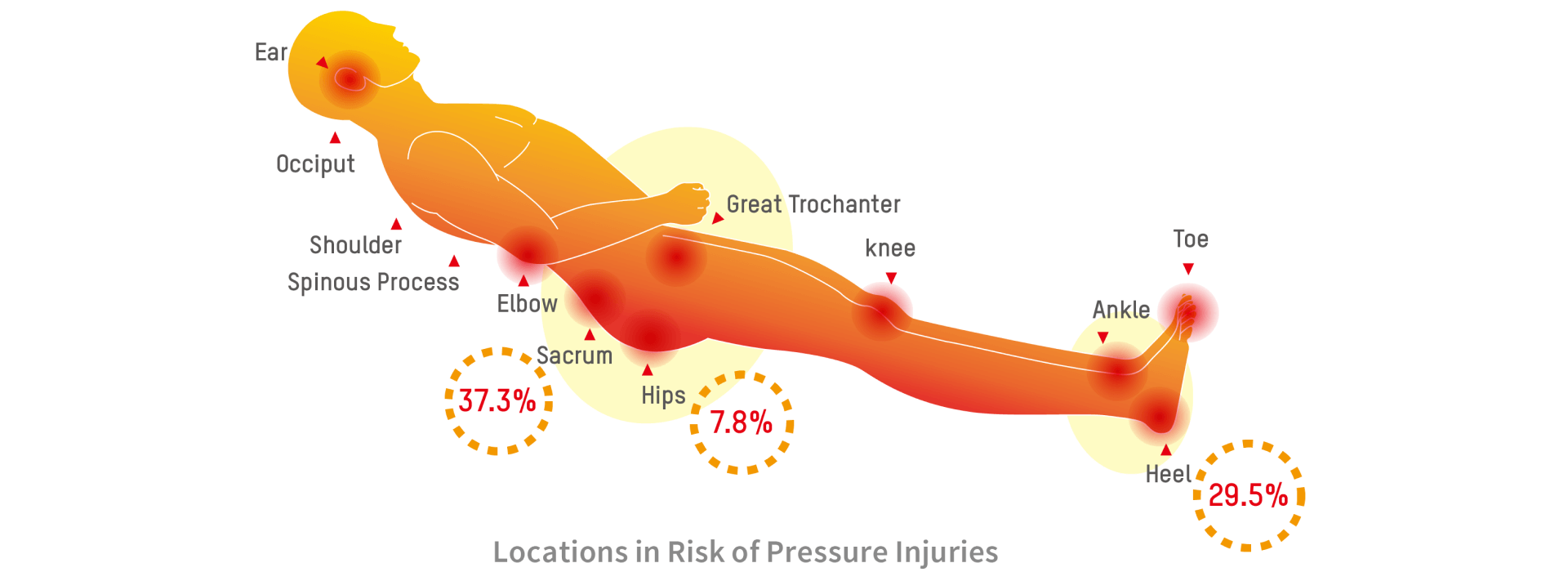
They may be superficial injuries affecting the epidermis and dermis or they can extend into the subcutaneous tissues and involve muscle, tendon and bone. Pressure injuries typically occur over bony prominences with the lower trunk (sacrum, coccyx, trochanter and ischial tuberosity) and heels being the two most common anatomical locations.3,4
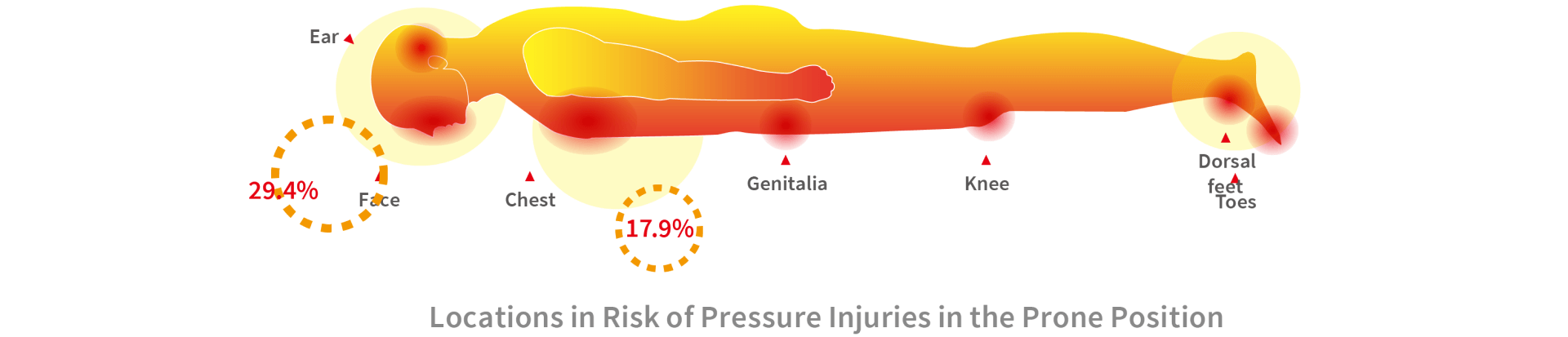
The prone position is related to a higher frequency of pressure injuries when comparing with the supine position.5 Locations like the face, ear, chest, genitalia, knees, dorsal feet and toes are at high risk when patients are positioned in the prone position.5,6
Localized areas of tissues that have prolonged pressure cause the occlusion of blood flow, preventing the supply of nutrients and oxygen to the tissue, resulting in ischaemia and re-perfusion injury, leading to cell obliteration and eventually tissue death.7
From the information of the mechanism of pressure injuries above, additional risk factors that have been correlated with are age of 70 years and older, current smoking history, dry skin, low body mass index, impaired mobility, altered mental status (i.e., confusion), diabetes mellitus, peripheral vascular disease, urinary and fecal incontinence, malnutrition, physical restraints, malignancy, history of pressure injuries, and human race.
Pressure injuries can develop within 2 to 6 hours. Therefore, the key to preventing pressure injuries is to accurately identify at-risk individuals quickly, so that preventive measures may be implemented.8 A major method of redistributing pressure is the use of support surfaces. Many researches had been conducted on the effectiveness of the use of support surfaces in reducing the incidence of pressure injuries. The concept of pressure redistribution has been embraced by the NPIAP.
“Support surfaces are: “Specialized devices for pressure redistribution.”9
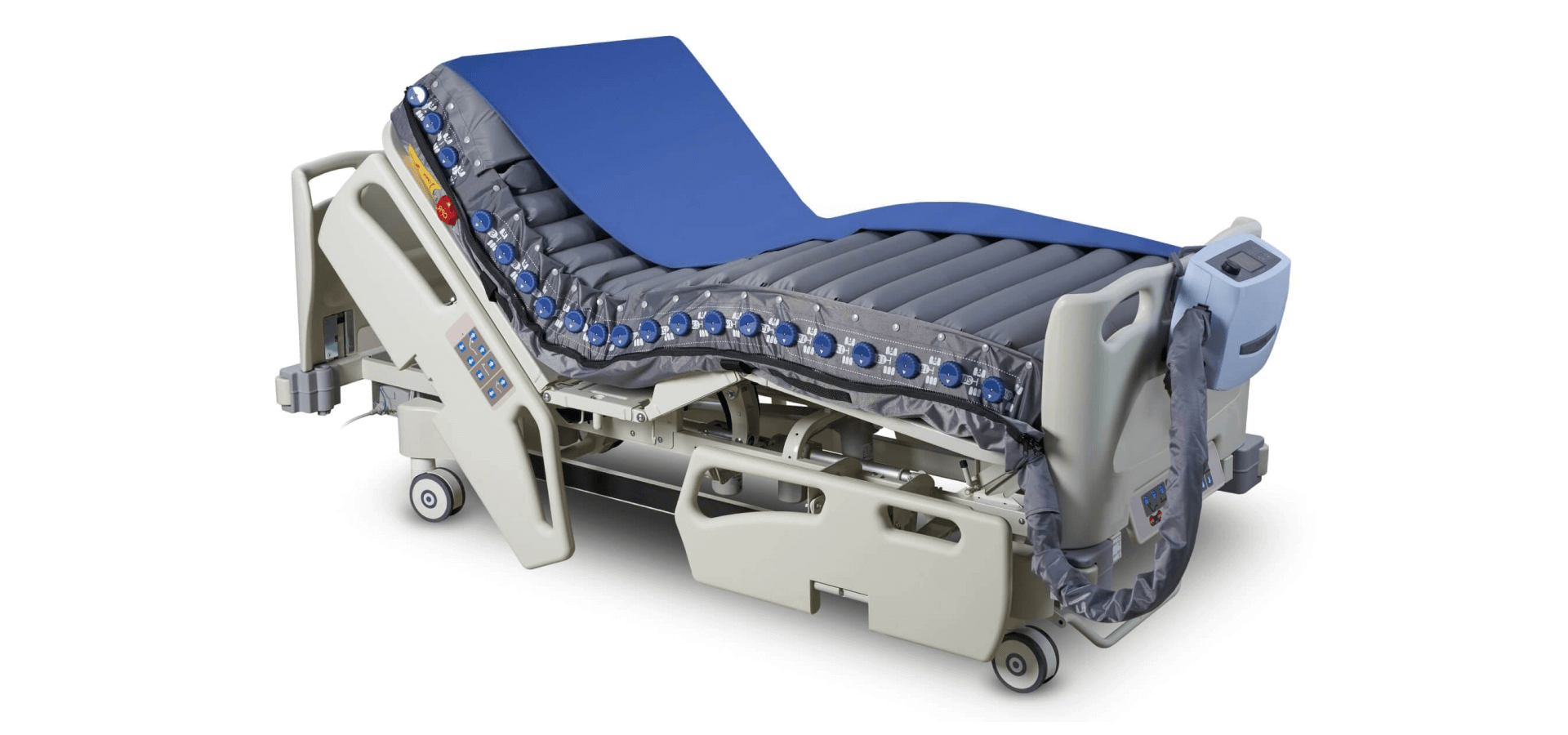
“Support surfaces are specialized devices for pressure redistribution designed for management of tissue loads, microclimate, and/or other therapeutic functions (i.e., any mattress, integrated bed system, mattress replacement, overlay, or seat cushion, or seat cushion overlay).”9 In this context, pressure refers to the distribution of force on the individual’s body surface that is in contact with the device.
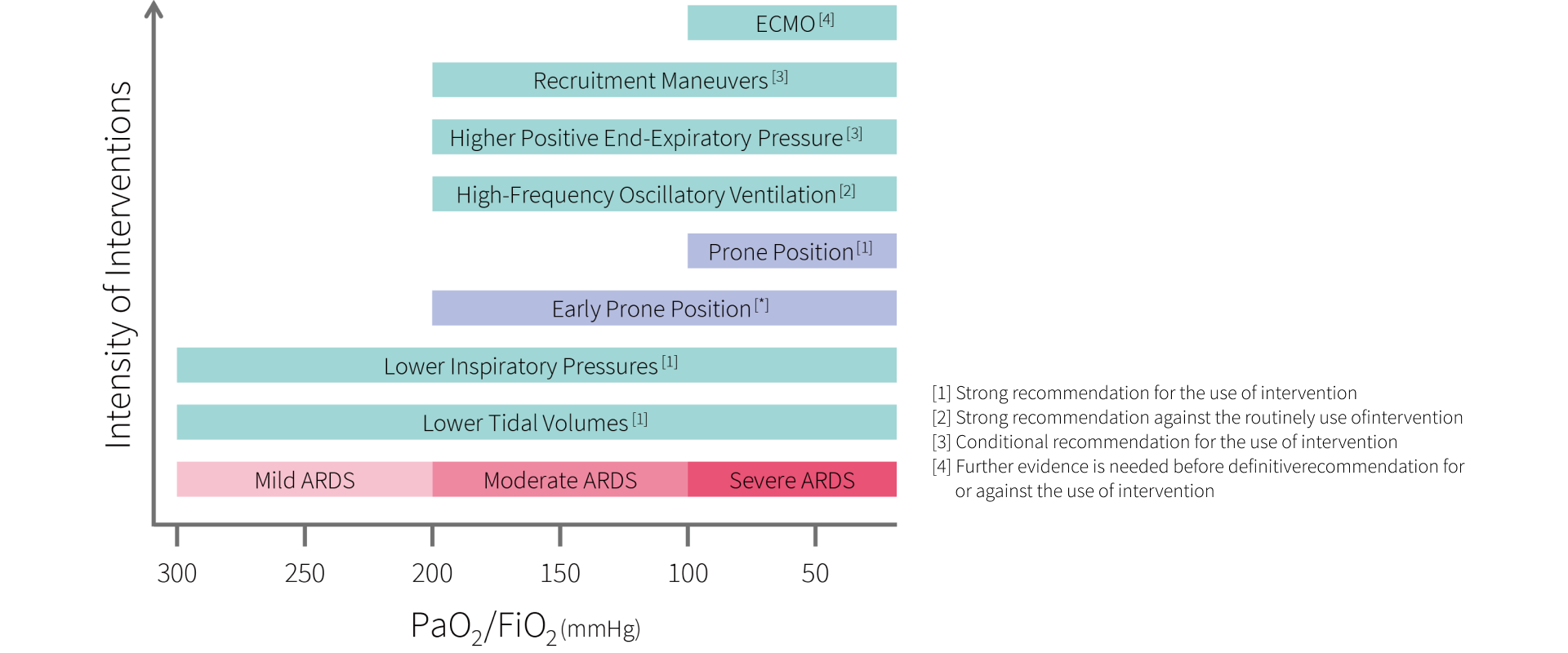
Acute respiratory distress syndrome (ARDS)
Acute respiratory distress syndrome is a type respiratory failure with mortality rates around 35% to 45% based on its severity.10 Based on the Berlin Definition, PaO2/FiO2 ratio is an indicator of hypoxemia and used to classify ARDS into 3 categories by the severity of hypoxemia.11
Definition & classification
| PaO2/FiO2 | 201 – 300 mmHg | 101 – 200 mmHg | ≤ 100 mmHg |
|---|---|---|---|
| ARDS | Mild | Moderate | Severe |
| Mortality | 27% | 32% | 45% |
(PaO2: arterial oxygen partial pressure; FiO2: fractional inspired oxygen)
Mechanism
Injury to the lungs increases permeability of lung endothelium and results in oedema in the lung interstitium. Then, the breakdown of alveolar epithelium leads to translocation of fluids into the alveoli. The hallmark of ARDS is the accumulation of fluid, proteins, neutrophils and red blood cells in the alveolar space. Ventilation perfusion mismatch (V/Q mismatch) and pulmonary shunt are the major causes to hypoxemia.11
Causes of ARDS
Bacterial, viral or fungal pneumonia, non-pulmonary sepsis, pulmonary aspiration, trauma such as penetrating or blunt injuries to the lungs and other serious illness are associated with the development of ARDS.10, 12
Mechanical ventilation with ARDS
According to the guideline on Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome published by The American Thoracic Society (ATS), European Society of Intensive Care Medicine (ESICM) and Society of Critical Care Medicine (SCCM), we summarized the recommendation of different interventions based on their severity.13 Early prone position is also recommended in moderate or severe ARDS patients.14-18
Prone position ventilation
“Use a pressure redistribution support surface or positioning devices to offload pressure points on the face and body while in the prone position.”19
“Avoid extended use of prone positioning unless required for management of the individual’s medical condition.”20
Prone positioning of patients was used in 16.3% (119 out of 729 patients) of patients with severe ARDS based on an international, multicenter, prospective cohort study.21 By positioning patients in the prone position will increase gas exchange and oxygenation.5, 10, 22 Patients’ mortality rate was significantly lower in the prone position when comparing to the supine position. Prone positioning of patients may improve their survival rate but it may also increase the incidence of pressure injuries.5 Therefore, prevention of pressure injuries in susceptible areas is important.
| Supine | Prone | ||
| Blood flow | Ventral lung | Minor | Major |
| Dorsal lung | Major | Minor | |
| Alveoli | Ventral lung | Overexpansion | Decrease overexpansion |
| Dorsal lung | Collapsed | Decreased collapsed | |
| V/Q | Mismatch | Better match |
Table 1. Physiology differences of supine and prone position in acute respiratory distress syndrome
Supine position vs prone position in ARDS patients23
Ventilation perfusion mismatch or V/Q mismatch is seen in patient lying in supine position, meaning one or more areas of the lung receive blood flow but no oxygen or they receive oxygen but lack blood flow. Placing patient in prone position can change the mechanics and physiology of gas exchange to improved oxygenation (Table 1, Table 2).
Contraindications to prone position ventilation
instability, open chest post cardiac surgery/trauma, unstable fractures especially facial or pelvic, anterior burns, pregnancy, conditions associated with raised intracranial pressure, etc.24
Prone position guidance
Guidance for: Prone Positioning in Adult Critical Care, published by The Intensive Care Society and the Faculty of Intensive Care Medicine (FICM), provides an example of safe and effective practice. For detail instructions, please refer to the original publication.25
| Supine position | Prone position | |
| Alveolar expansion | The nondependent alveoli (ventral alveoli) are more distended than the dependent alveoli (dorsal alveoli). This is likely exaggerated especially in ARDS patients when placed in the supine position due to increase of lung weight. | In the prone position, not only can it lower overexpansion of the ventral alveoli but also decrease collapse of the dorsal alveoli. |
| Lung compression | In the supine position, the heart and the diaphragm compress the lungs and lead to collapse of the dependent lung. | The heart lies on the sternum and the diaphragm is displaced caudally. Compression of the lung is decreased. |
| Lung perfusion | Collapse of alveoli and blood flow are at most in the dependent region of lung causing a ventilation perfusion mismatch (V/Q mismatch) phenomenon. | Ventilation perfusion match is better since the alveoli in the former dependent region of the lung begin to expand and still receive the greater part of the blood flow. On the other hand, the alveoli in the newly dependent region of the lung start to collapse while receiving the less part of the blood flow. |
Table 2. Physiologic effects on oxygenation
Optima Prone features
Supporting prolong pressure relief
 Continuous Low Pressure (CLP)
Continuous Low Pressure (CLP)
 Alternating Mode
Alternating Mode
 Multi-zone Air Pressure
Multi-zone Air Pressure
 Auto Seat Inflation
Auto Seat Inflation
 Supine Position Mode & Prone Position Mode (with Prone Position Timer)
Supine Position Mode & Prone Position Mode (with Prone Position Timer)
 Individual Air Cell Deflation (including Heel Relief Function)
Individual Air Cell Deflation (including Heel Relief Function)
 Shoulder Lifting Mode
Shoulder Lifting Mode
 Head Reposition Mode - Single-Caregiver Operation
Head Reposition Mode - Single-Caregiver Operation
 Pressure Redistribution in the Head Section
Pressure Redistribution in the Head Section
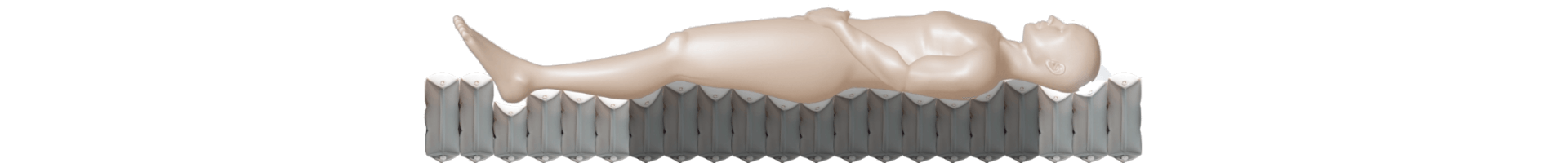
 QubiCellTM Design
QubiCellTM Design
Improving protection against friction & shear
 4-way Stretch Top Cover with Low Friction & High MVTR
4-way Stretch Top Cover with Low Friction & High MVTR
Alleviating moisture & heat
 Micro Low Air Loss
Micro Low Air Loss
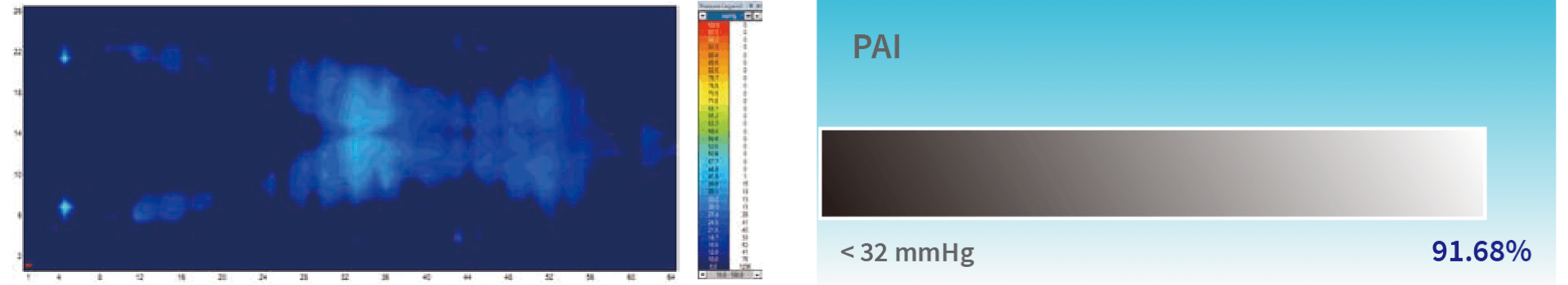
Pressure mapping
By investigating the pressure mapping of Optima Prone, we can use the software to analyze the Pressure Area Index (PAI) and Pressure Redistribution Index (PRI) of different modes to see the performance of product, when threshold of interface pressure gets stricter, you can find out that Optima Prone can still offer good performance for prevention of pressure injuries.
Equipment used: The XSENSOR X3 Display Medical Mattress System
Software used: Xsensor X3 medical V6
*No. 9 & 11 cells were deflated in the torso section and No. 20 ~ 21 cells for the lower leg section when testing in prone position. For more information, please refer to the Individual Air Cell Deflation section.
Pressure Area Index (PAI): Pressure Area Index (PAI) is a method used to measure the interface pressure of the surface. The PAI is calculated as the proportion of sensors that register interface pressure values.26
Pressure Redistribution Index (PRI): Pressure Redistribution Index (PRI) is a method to assess the ability of a dynamic support surface to sustain interface pressures below a chosen set of thresholds. The PRI is calculated as the ratio of the time during which the dynamic support surface interface pressure trace spends below the threshold and the total time of one inflation/deflation cycle.27
Product therapy modes and performance
Initial inflation
Once the pump recognizes the mattress size through the quick connector, it will begin to inflate mattress which takes less than 30 minutes to complete the initial inflation.

Continuous low pressure (CLP)
“Consider using a reactive air mattress or overlay for individuals at risk for developing pressure injuries.”28
Reactive air mattresses redistribute pressure by deforming in response to an individual’s weight on the surface.29 Optima Prone offers a Continuous Low Pressure mode, which provides a stable surface with a pressure lower than the corresponding level when in the alternating mode. Also, this therapy mode is for the patients who are not fond of vibrations or alternating sensations.
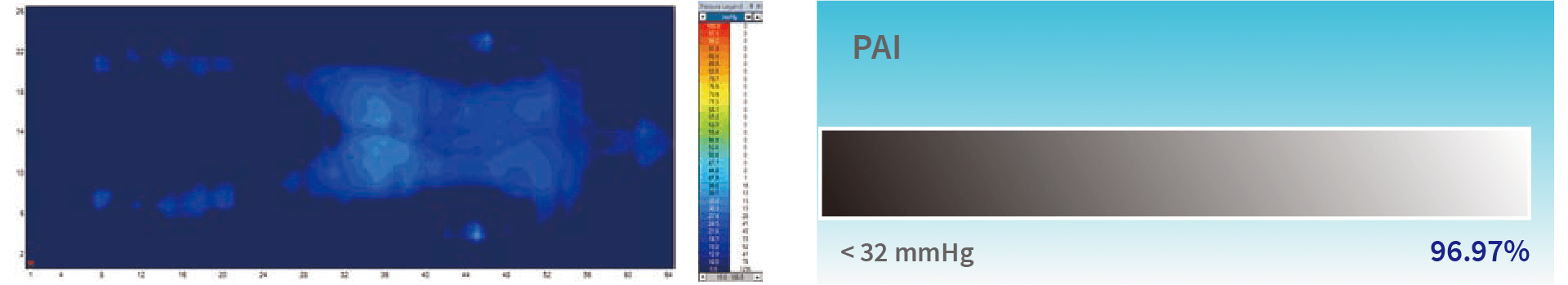
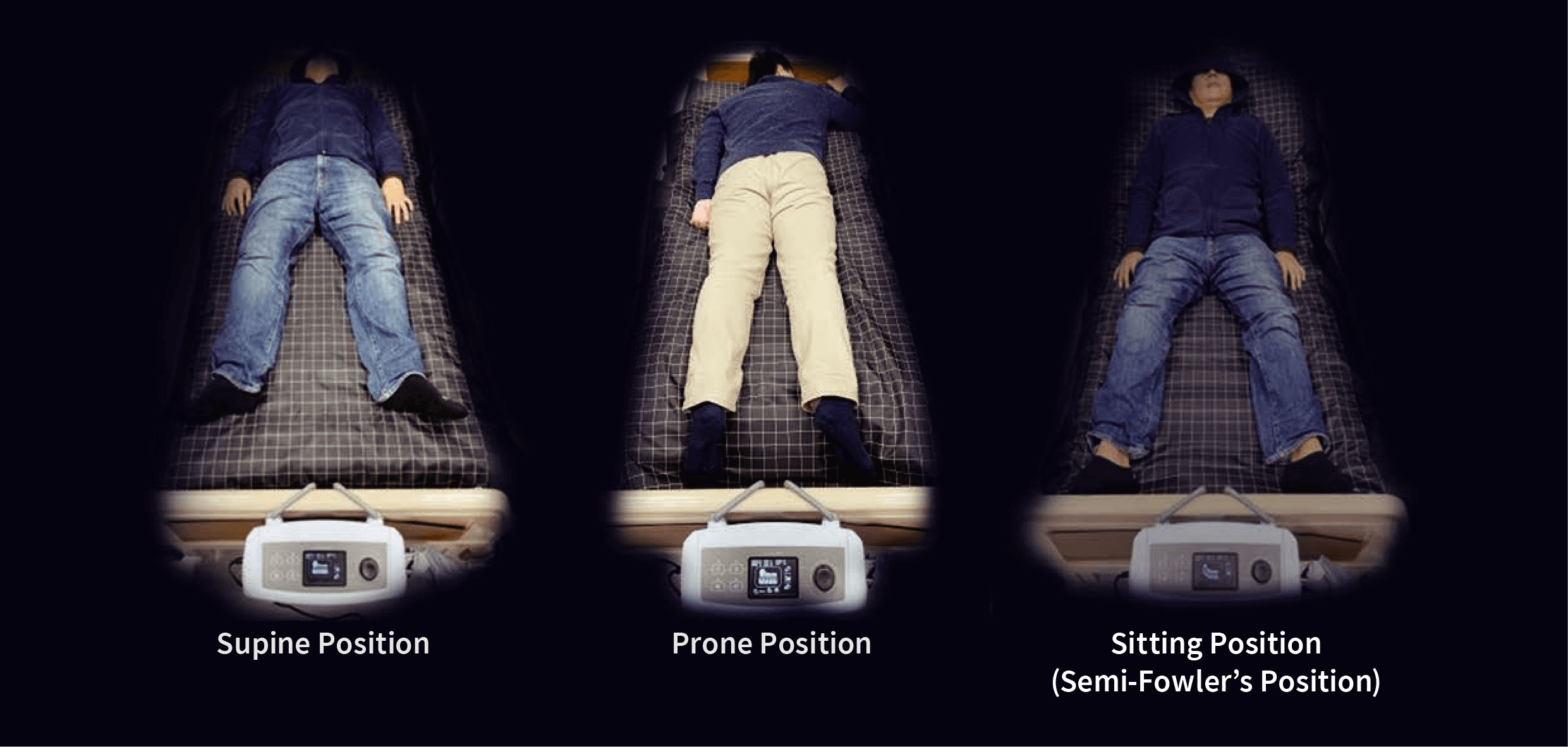
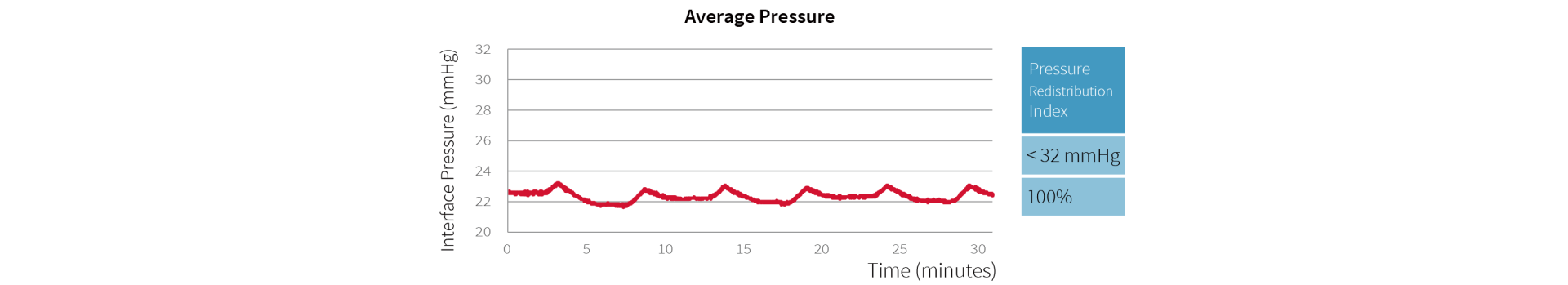
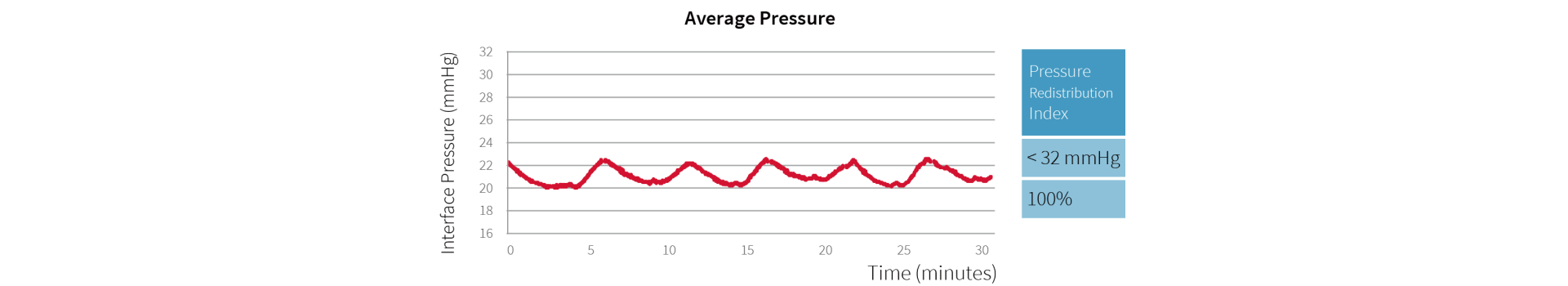
Supine Position: PAI & Pressure Mapping test of Optima Prone in the supine position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
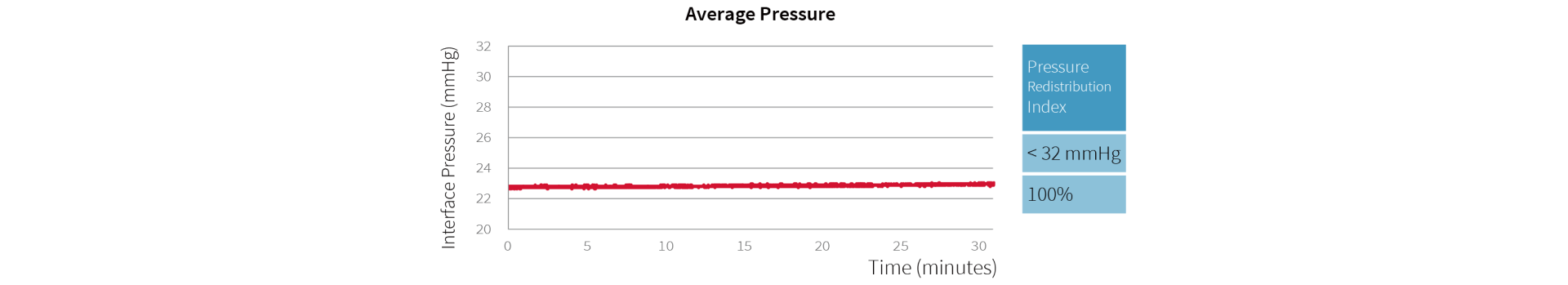
Optima Prone (when used in Continuous Low Pressure mode) reaches a maximum of 20.1 mmHg and a minimum of 19.6 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
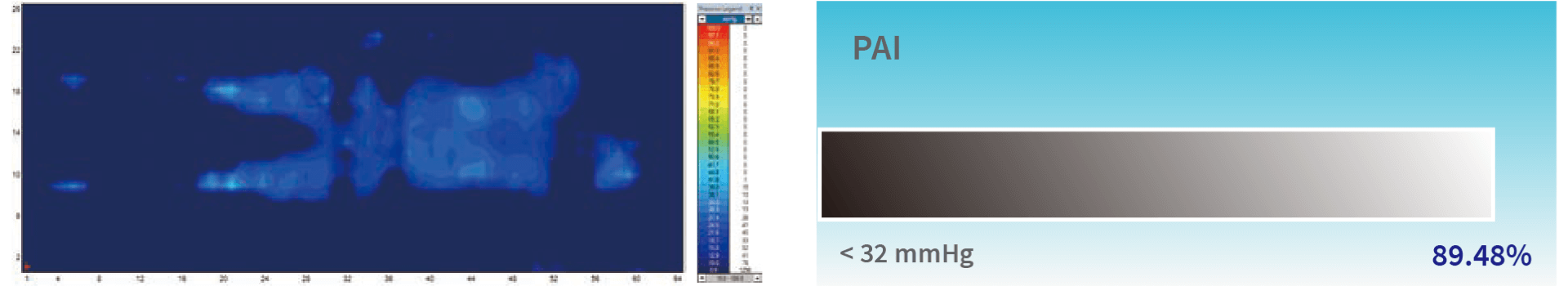
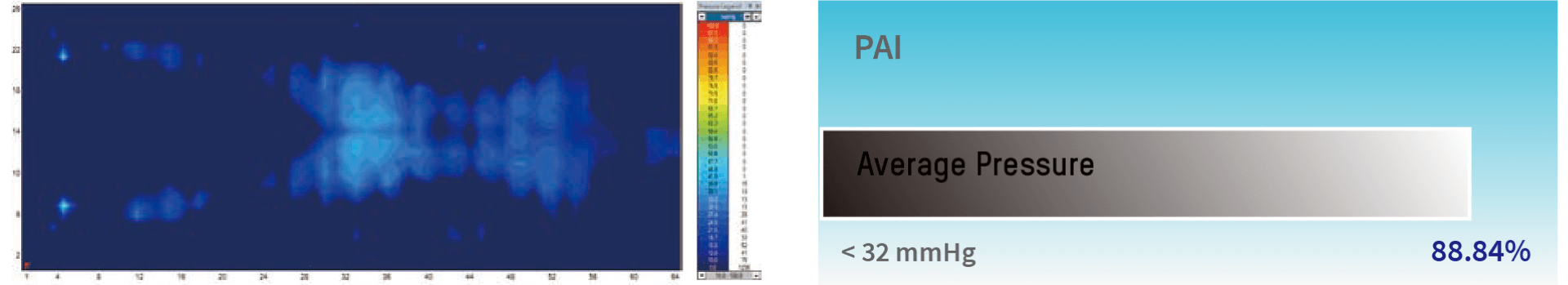
Prone position: PAI & Pressure Mapping test of Optima Prone in the prone position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
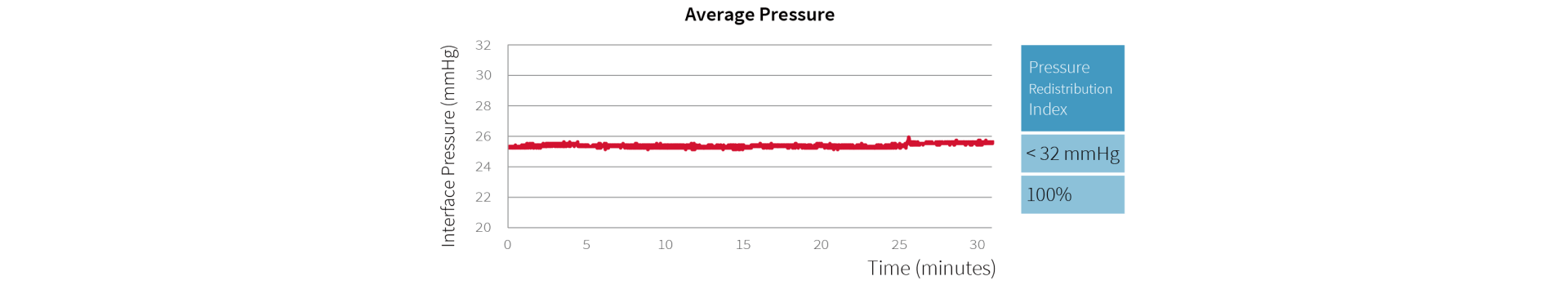
Optima Prone (when used in Continuous Low Pressure mode) reaches a maximum of 26.2 mmHg and a minimum of 25.4 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
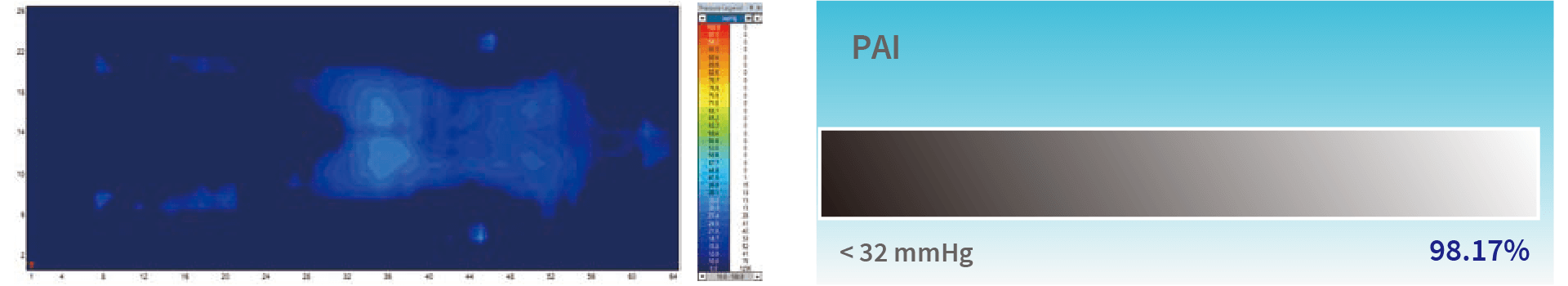
Sitting position: PAI & Pressure Mapping test of Optima Prone in the sitting position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
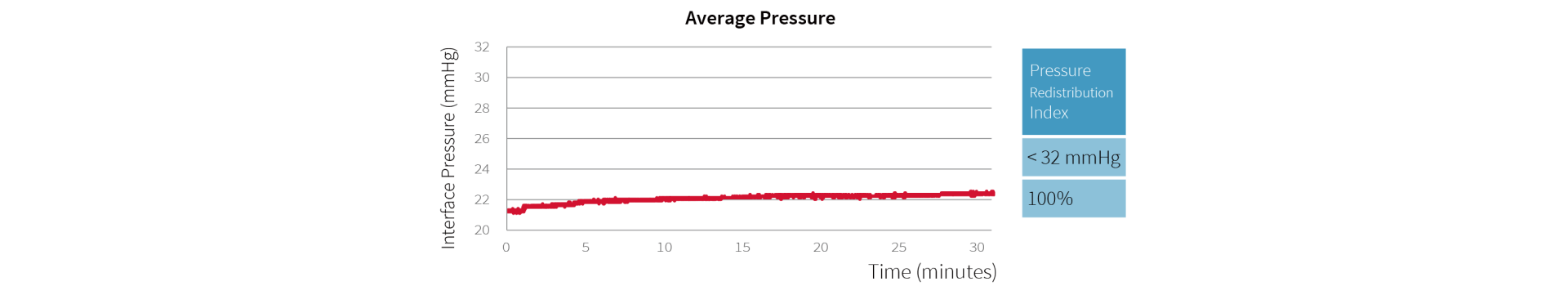
Optima Prone (when used in Continuous Low Pressure mode) reaches a maximum of 22.4 mmHg and a minimum of 21.0 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
Alternating mode
“Assess the relative benefits of using an alternating pressure air mattress or overlay for individuals at risk of pressure injuries.”30
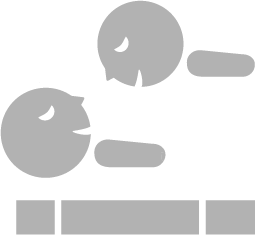
Optima Prone offers an alternating mode, which continuously and sequentially inflate and deflate air cells (1-in-2 alternating) to avoid long term pressurization of tissue, and also provides four kinds of operating cycle time (10, 15, 20, 25 min).
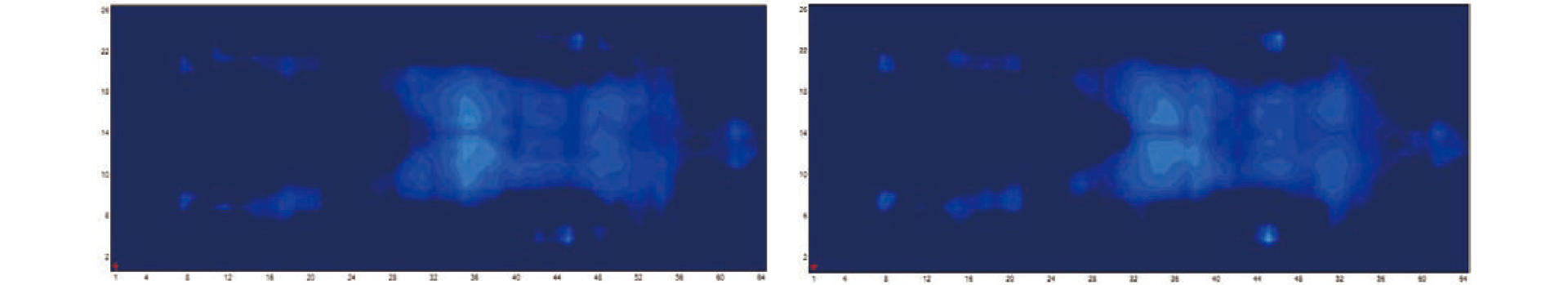
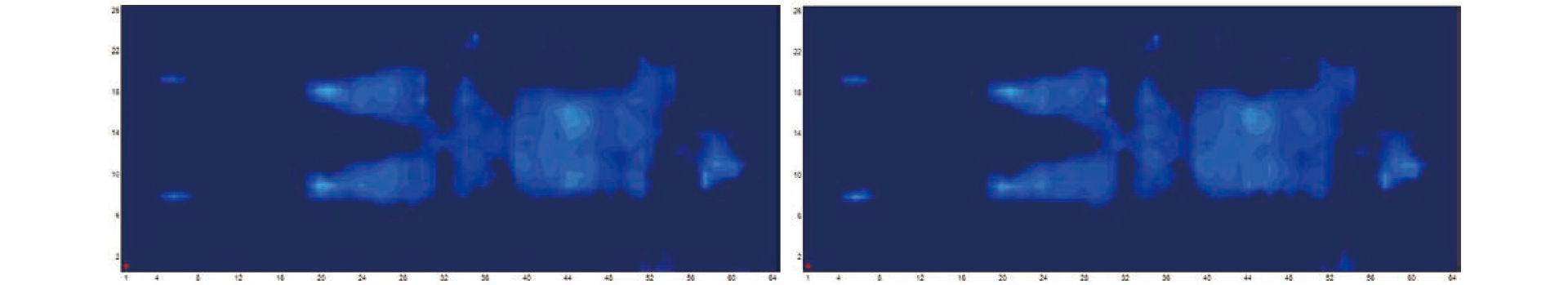
Supine position: PAI & Pressure Mapping test of Optima Prone in the supine position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
Optima Prone (when used in alternating mode) reaches a maximum of 20.3 mmHg and a minimum of 18.2 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
From the pressure mapping images you can easily observe the alternating situation in the supine position:
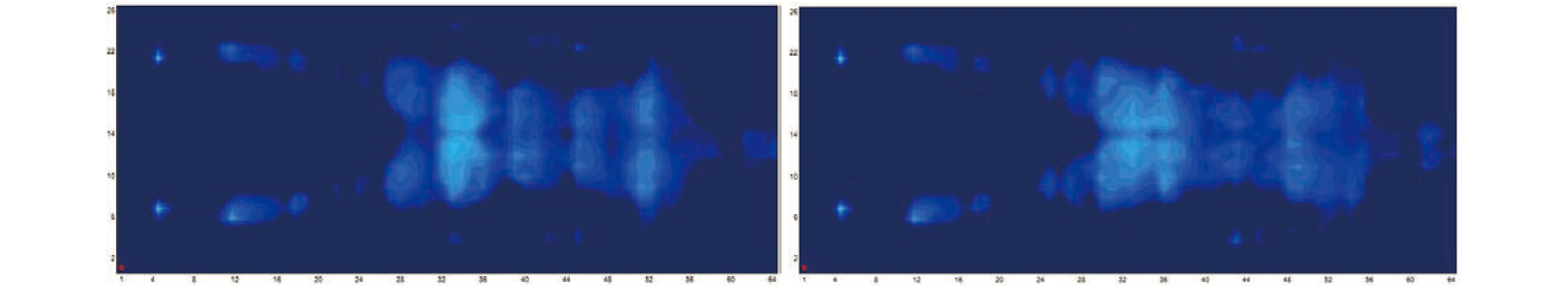
Prone position: PAI & Pressure Mapping test of Optima Prone in the prone position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
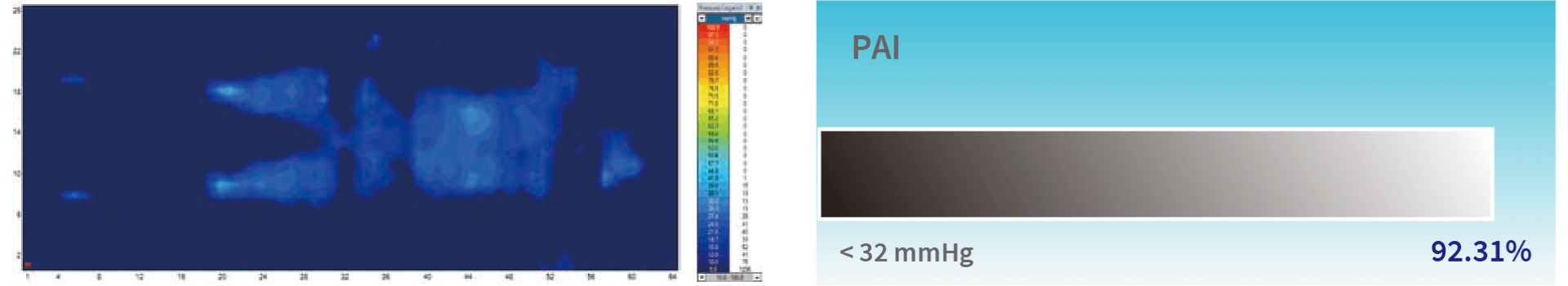
Optima Prone (when used in alternating mode) reaches a maximum of 26.6 mmHg and a minimum of 24.3 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
From the pressure mapping images you can observe the minor alternating situation in the prone position. The reason for minor alternating is to provide better support and comfort for patients lying on their stomach:
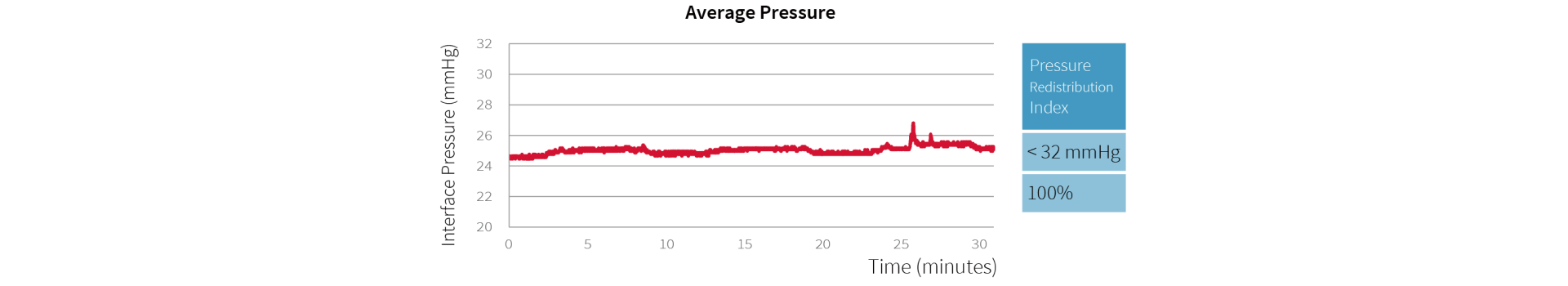
Sitting position: PAI & Pressure Mapping test of Optima Prone in the sitting position for 30 min. User height 177 cm, user weight 90 kg, and BMI 28.73.
Optima Prone (when used in alternating mode) reaches a maximum of 22.6 mmHg and a minimum of 20.0 mmHg, and the 100% of interface pressures during its 30 minute cycle are all below 32 mmHg.
From the pressure mapping images you can easily observe the alternating situation in the sitting position:
Multi-zone air pressure
“Pressure redistribution is achieved by either increasing the body surface area that comes in contact with the support surface through immersion and envelopment (to reduce concentrations of weight over bony prominences).”31
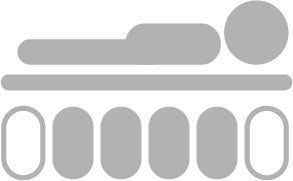
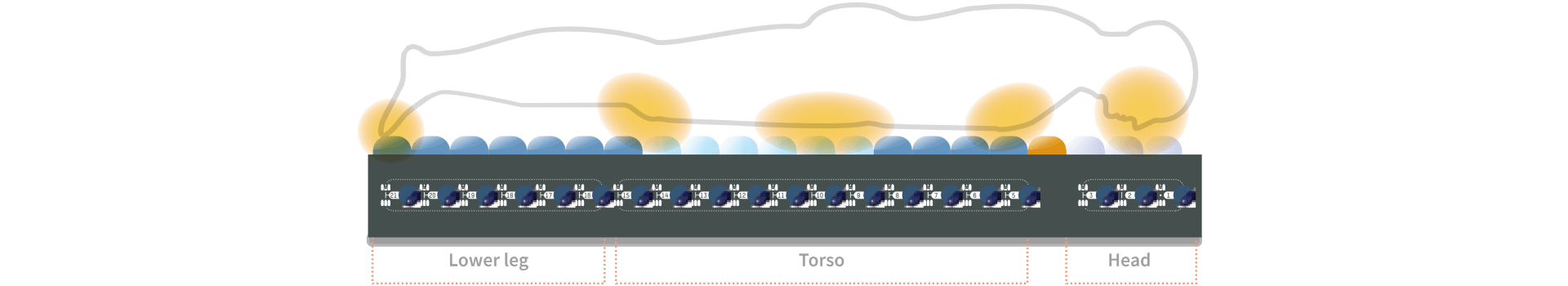
In consideration of the body segment mass and anatomical structures, the mattress of Optima Prone is divided into three zones: Head, torso and lower leg.
Torso accounts for more than 40% of the body weight and areas such as scapula, sacrum, and hip are susceptible to pressure injuries.
Multi-zone Air Pressure demonstrates significant pressure redistribution to fit different patient contours with stability and comfort by better immersion and envelopment.
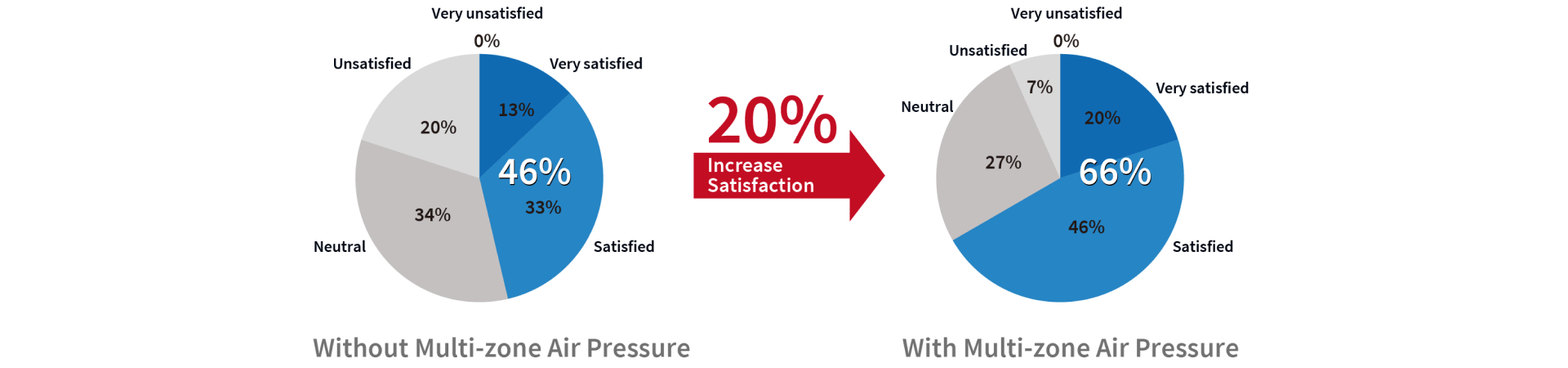
An in-house single-blinded test was done to evaluate the comfort level that Multi-zone Air Pressure offers to the participants.
73% (11 out of 15 users) would prefer the optimal comfort Multi-zone Air Pressure provides. In addition, there was a 20% increase in satisfaction percentage showing the comfort level was relatively higher in mattress with Multi-zone Air Pressure.
Auto seat inflation
“For individuals with a pressure injury, consider changing to a specialty support surface when the individual: ‘Bottoms out’ on the current support surface.”36
To avoid the situation of bottoming out, Optima Prone offers an Auto Seat Inflation function, which automatically inflates when the head section has been raised by ≥ 30°, and provides extra support in sacral area during sitting position. The pressure in the whole mattress increases when the patient is in a fowler’s position for a steady support. Optima Prone is also equipped with 6 Cell-in-Cell air cells at sacrum area, by which provide excellent support for the patient in sitting-up position or when exiting and entering the mattress.

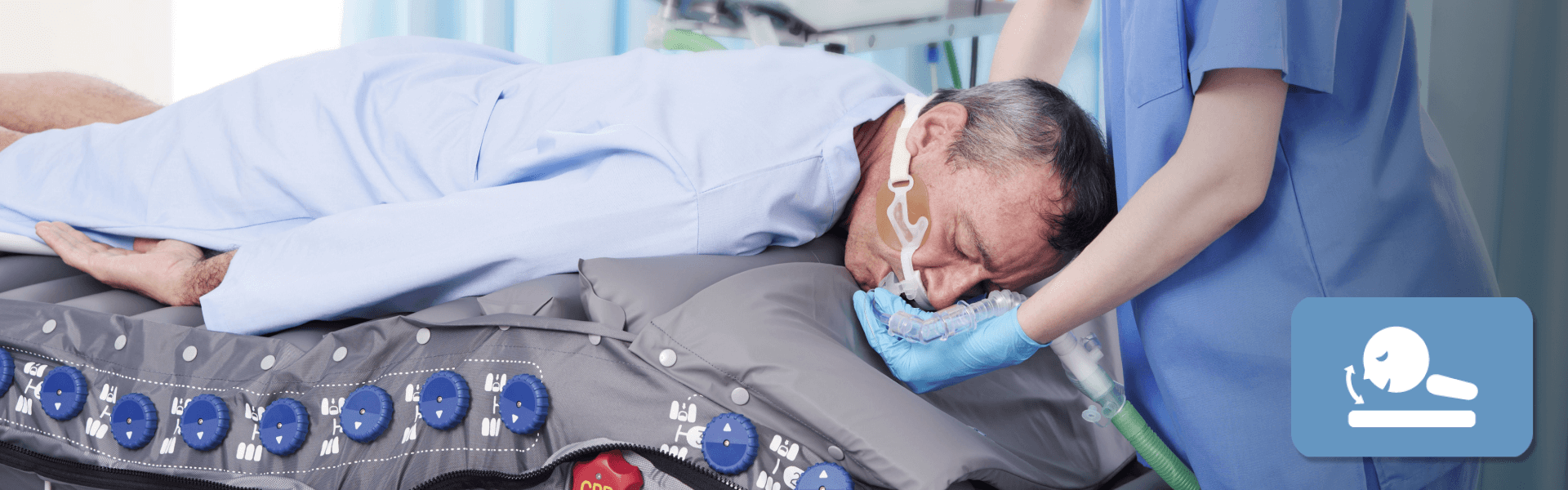
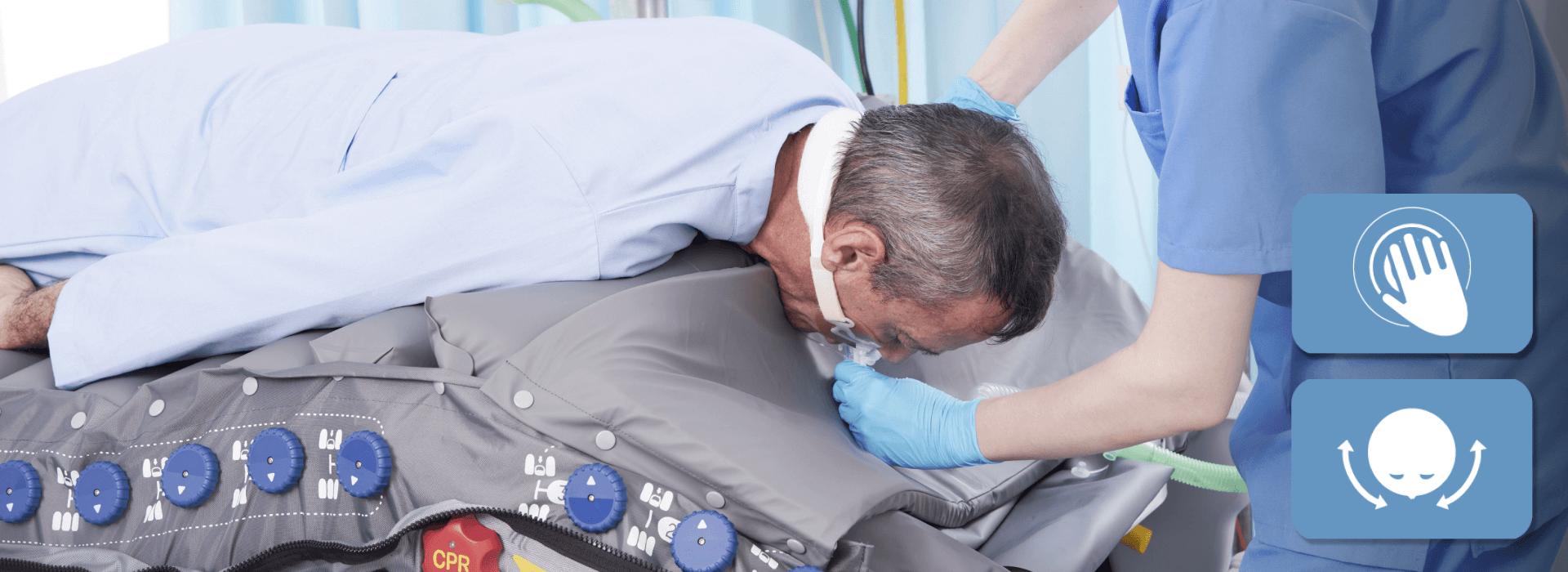
CPR Operation
CPR knob is located at the patient’s left-hand side of the mattress near the head section area. Whenever a CPR operation is needed, quickly turn the CPR knob to release air from the mattress. The CPR deflation time is within 15 seconds. The quick connector on the pump unit can be disconnected for an even faster deflation process.

Design of mattress
Supine position mode & prone position mode
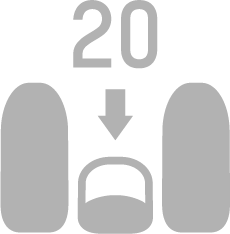
Optima Prone offers two modes for different positions: Supine Position Mode & Prone Position Mode. Before turning the patient, select a mode and Max Firm will be activated automatically to provide a stable surface for turning pro cedures which last for 20 minutes.

Prone position timer
Prone ventilation for 12–16 hours per day is recommended in patients with severe ARDS.37 Once you selected the Prone Position Mode, it will start the timer automatically to show caregivers how long the patient have been positioned in prone position.

Individual air cell deflation
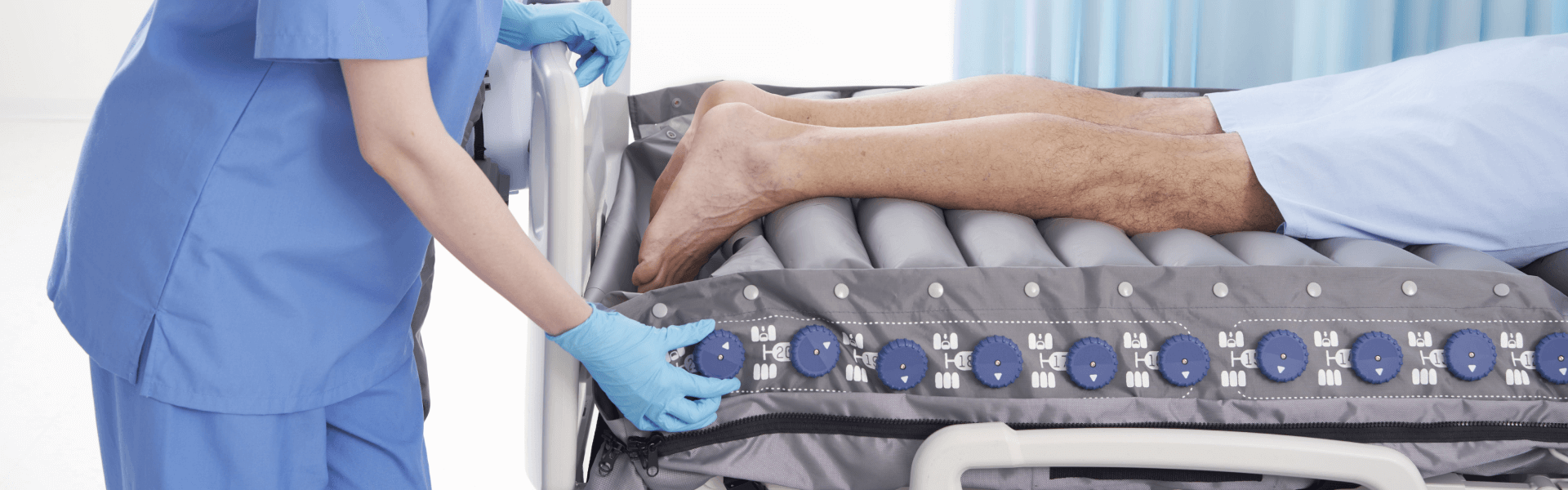
One-handed control knobs (which have been designed for helping prevention of cross infection) along the side of the mattress allow individual cells to be deflated. The only exception is the 4th air cell which aims to support the shoulders.
The knobs are numbered from 1 to 21 and are split into 3 sections: Head, Torso and Lower leg.
Completely deflate cells according to patient’s vulnerable areas either in the supine or the prone position.
Based on these areas, we recommend you deflate:
- 2 cells in the Torso section (No. 5 – 15), 1 at the abdomen to increase ventilation or 1 at the chest to reduce pressure and 1 at the groin to ensure no compression to the urinary catheter.
- 1 cell in the Lower leg section (No. 16 – 21) to achieve zero pressure to the heels (supine position) or dorsal feet and toes (prone position).
- 1 cell in the Head section (No. 1 – 3) when the patient is placed in the supine position or 3 cells in the Head section when repositioning the patient’s head in the prone position.
Aside from the therapy needed, we highly recommended not to deflate any more cells we mentioned above to ensure the support of the patient.
Heel relief function
“The heel is one of the two most common anatomical sites for pressure injuries. In a European survey on pressure injury prevalence, almost 80% of all Category/Stage IV pressure injuries were found at the sacrum and heels.”33
Optima Prone is also equipped with Heel Relief Function which is a simple and easy way to prevent and assist in treating heel pressure injuries by eliminating interface pressure from heels as if they are suspended in air. The heel is typically reported as the second most common sites for pressure injury development.33
One of the six knobs in the lower leg section can be deflated according to the patient’s heel location to achieve zero pressure.
Shoulder lifting mode
Pillows if required, can be placed over the chest, iliac crests and knees.” The purpose of placing pillow across patient’s chest is to allow breasts to be supported and free from pressure.25
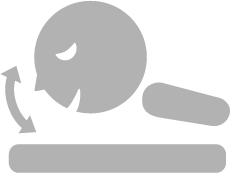
Once Shoulder Lifting Mode is selected, the air cell underneath the shoulder and chest section will start to inflate, releasing the neck pressure, avoiding spinal deformity, body pain and reduce the risk of hyperextension for patients in prone position. Two angles are provided according to the patient’ s need. (This mode will stay on once selected.) Two angles are provided according to the patient’s need.
Head reposition mode - single-caregiver operation
Reposition of the patient’s head every 2 to 4 hours is required for those in prone position to alleviate pressure.25 Before the following procedures, place patient’s both arms straight and alongside the body. There are two ways to reposition the head which are both labor-intensive which require at least 3 highly trained staff members:
1) It can be done by boosting the patient up to the head of the bed so that the head is floating off the mattress. Then, carefully reposition the head to the opposite side with the help of the other two staff. Slide the patient back down the bed so the head is supported by the mattress. It may create lots of friction and shear force during the process.25
2) The second way is to pull the patient’s chest upward by lifting the shoulders to reposition the head. Once Head Reposition mode is selected, the air cell underneath the 4th to 6th cells will start to inflate to lift the patient’s shoulders and chest upward. A short beep indicates the mattress is now stable for the following procedures.
This mode will last up to 10 minutes and will return to the previous setting automatically. It can also be canceled manually.
Optima Prone enables single-caregiver operation when repositioning patient’s head regularly when in prone position. With the support of Individual Air Cell Deflation and Head Reposition Mode, deflation of the head section air cells and elevation of the patient’s shoulders and chest help repositioning the patient’s head easier by one person.
Pressure redistribution in the head section
“Use a pressure redistribution support surface or positioning devices to offload pressure points on the face and body while in the prone position… Individuals placed in the prone position may be at increased risk for the development of facial pressure injuries.”19
Head section of Optima Prone provides gentle support of the head. Alternating mode, the 3 head section cells along with the rest of the cells alternate to provide pressure relief of the head in prone position and also protect the occiput, which is also susceptible to pressure injuries in the supine position. A special foam design helps prevent pressure injury to the patient’s ears by achieving zero pressure to the ear when being positioned in swimmer’s position. This design is based on the CAESAR database for human ear size.38
QubiCellTM
“Use a pressure redistribution support surface or positioning devices to offload pressure points on the face and body while in the prone position… Individuals placed in the prone position may be at increased risk for the development of facial pressure injuries.”19
Optima Prone consists of 21 rectangular cells, providing a larger contact area and thus lower interface pressure in either supine or prone position.
Thanks to its solenoid valve technology, it can enable more stable & comfortable alternating cycles - it inflates odd air cells before deflating even air cells (and vice-versa) during the alternating process by turning the valves on and off sequentially to provide an effective therapy in high comfort for the patient>
TPU air cells & air cell holder design
Thermoplastic polyurethanes (TPU) air cells used for Optima Prone mattress are highly resistant to hydrolysis, soft, less friction and even less noisy when patient is moving their body on the mattress, its material chose and the design of the air cell holders are in aids with reducing friction & shear forces for the patient lying in different postures.

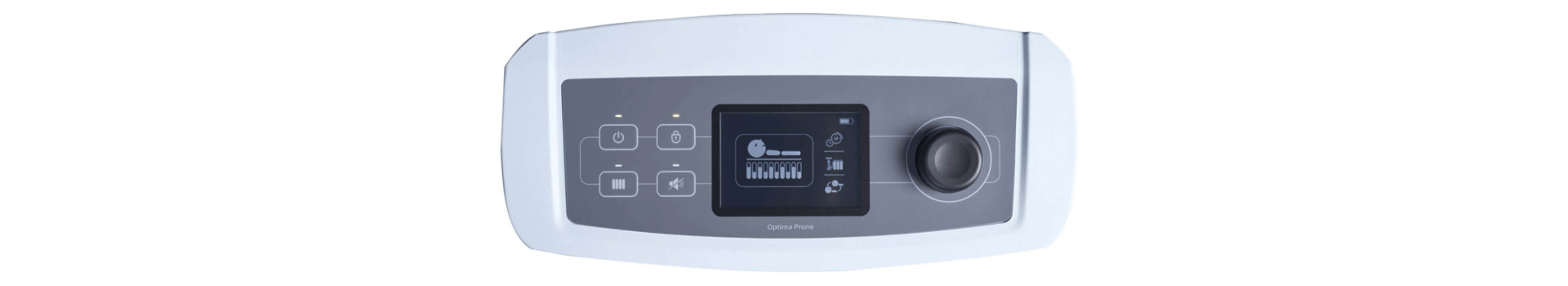
LCD monitor
Optima Prone pump is equipped with a control knob without grooves (which has been designed for helping prevention of cross infection) and a LCD screen with an intuitive graphic design to save time and effort for operation and troubleshoot, reducing the chance of misuse.
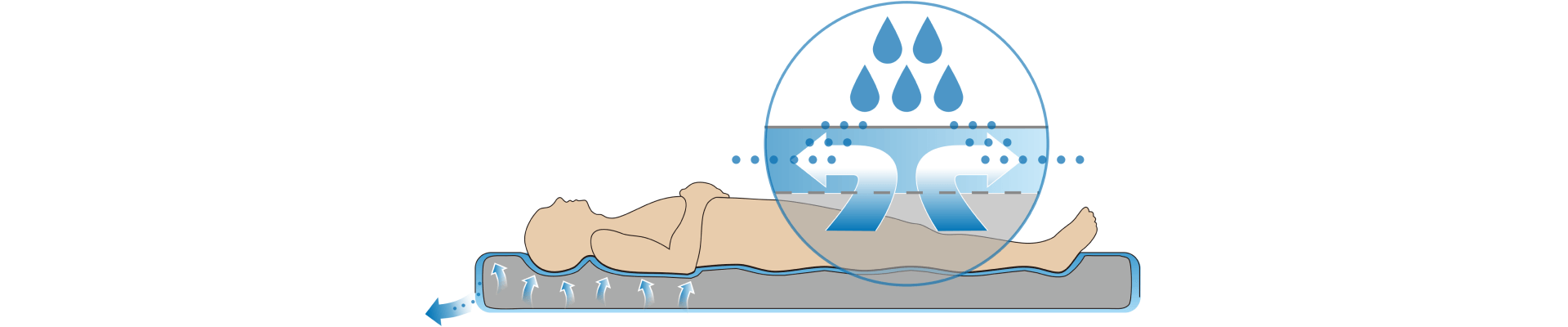
Top cover
“Consider using textiles with low friction coeAcients for individuals with or at risk of pressure injuries.”39
Optima Prone alternating pressure redistribution system is provided with a standard cover (sanitary cover sheet) with high-performance technical material which covers them completely and is biocompatible, with low friction (μ = 0.21 (static), μ = 0.17 (dynamic)) & shear forces, water resistant and highly vapor permeable.
The Moisture vapor transmission rate (MVTR) is 2315 g/24hrs/m2 according to ASTM E96 Procedure BW.

Microclimate management
“An increasing body of evidence suggests that the microclimate between skin and the supporting surface plays a role in the development of pressure injuries.”40
As for the microclimate control, Optima Prone offers micro low air loss function, which provides good ventilation and reduces the accumulation of heat and moisture.
Transport mode (built-in battery) (optional)
“Contingency plans for power failure should be in place.”41
The Optima Prone with optional battery pack can offer a nonstop dynamic pressure relief for up to 6 hours in addition to the 24 hours the standard mattress system can remain inflated during power failure or patient transfer.

Design of saving time
The air cells with quick release detachable base on Optima Prone can be easily removed from mattress during decontamination which can save up to 80% of time compared to regular mattress systems.
Optima Prone is also equipped with a cable management feature which can reduce tripping hazards for a safer healthcare environment.
Frequently Asked Questions (FAQ)
During the 20-minute Max Firm after selecting either Supine Position Mode or Prone Position Mode, will Optima Prone conduct automatic detection of patient weight and provide corresponding pressure to optimize mattress pressure relieving performance?
No, during this period of time, Automatic Pressure Adjustment will not be activated.
What are the recommended numbers of cells you can deflate in each section for the Individual Air Cell Deflation? How to achieve Heel Relief Function?
Completely deflate cells according to patient’s vulnerable areas either in the supine or the prone position.
Based on these areas, we recommend you deflate: 2 cells in the Torso section (No. 5-15), 1 cell in the Lower leg section (No. 16-21), and 1 cell in the Head section (No. 1-3) when the patient is placed in the supine position or 3 cells in the Head section when repositioning the patient’s head in the prone position.
There are six knobs in the lower leg section, which can be accessed to deflation of air cells according to the patient’s heel location to achieve zero pressure.
What is the purpose of Shoulder Lifting Mode?
By lifting the patient’s shoulders and chest upward, it helps releasing the neck pressure, avoiding spinal deformity body pain and reduces the risk of hyperextension for patients in the prone position.
How long does the Head Reposition Mode remain activated?
Head Reposition Mode enables the caregiver to reposition the patient’s head easier by lifting the patient’s shoulders and chest upward. This mode will last up to 10 minutes and will return to the previous setting automatically. It can also be canceled manually.
How to enable Single-Caregiver Operation when repositioning patient’s head regularly while in prone position?
With the support of Individual Air Cell Deflation and Head Reposition Mode, deflation of the head section air cells and elevation of the patient’s shoulders and chest help repositioning the patient’s head easier by fewer people.
Selecting either Supine Position Mode or Prone Position Mode and Max Firm will be activated automatically to provide a stable surface for turning procedures which last for 20 minutes. After that, will it return to the previous therapy mode, i.e., Alternate mode?
Yes, it will return to the previous therapy mode automatically.
When patient is placed in prone position with several recommended air cells deflated, will it cause any risk of bottoming out under alternating mode?
No, the purpose of minor alternating is to provide better support and comfort for patients lying on their stomach.
There are no ventilated cells, why? Due to transport mode?
Micro Low Air Loss function was adjusted to the side of the mattress.
The Optima Prone with optional battery pack can offer a non-stop dynamic pressure relief for up to 6 hours in addition to the 24 hours the standard mattress system can remain inflated during power failure or patient transfer.
What is the material of air cells?
Thermoplastic Polyurethanes (TPU) Air Cell has high resistant to hydrolysis, soft, less friction and less noisy when patient is moving their body on the mattress.
What is the purpose of cell-in-cell air cells?
Optima Prone is also equipped with 6 Cell-in-Cell air cells at sacrum area, by which provide excellent support for the patient in sitting-up position or when exiting and entering the mattress.
What is the max patient weight of this product?
Optima Prone: 250 kg.
- Karen Hertz. 2018. Fragility Fracture Nursing. USA: Springer.
- NPIAP Pressure Injury Stages (https://cdn.ymaws.com/npiap.com/resource/resmgr/online_store/npiap_pressure_injury_stages.pdf).
- Zhaoyu Li, Frances Lin, Lukman Thalib, Wendy Chaboyer. 2020. Global prevalence and incidence of pressure injuries in hospitalized adult patients: a systematic review and meta-analysis. Journal of Nursing Studies.
- Gawlitta D, Li W, Oomens CW, Baaijens FP, Bader DL, Bouten CV. 2007. The relative contributions of compression and hypoxia to development of muscle tissue damage: an in vitro study. Annals of Biomedical Engineering. 35(2), 273-84.
- Girard R et al., 2014. The impact of patient positioning on pressure ulcers in patients with severe ARDS: results from a multicentre randomised controlled trial on prone positioning. Intensive Care Medicine.
- Section 8: Repositioning and Mobilization. Page 139
- Section 5: Skin and Tissue Assessment. Page 74
- International review. Pressure ulcer prevention: pressure, shear, friction and microclimate in context. A consensus document. London: Wounds International, 2010.
- Section 10: Support Surfaces. Page 155
- Dirkes S et al., 2012. Prone positioning: is it safe and effective? Critical Care Nursing Quarterly
- ARDS Definition Task Force. 2012. Acute Respiratory Distress Syndrome: The Berlin Definition. The Journal of the American Medical Association
- Matthay MA et al., 2019. Acute respiratory distress syndrome. Nature Reviews Disease Primers
- Laurent J. Brochard et al., 2017. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. American Journal of Respiratory and Critical Care Medicine.
- PROSEVA Study Group. 2013. Prone Positioning in Severe Acute Respiratory Distress Syndrome. The New England Journal of Medicine.
- Sachin Sud. et al., 2014. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Canadian Medical Association Journal.
- Bloomfield R et al., 2015. Prone position for acute respiratory failure in adults (Review). Cochrane Database of Systematic Reviews.
- Aline Almeida Gulart et al., 2020. Early prone position for COVID-19 patients with severe hypoxia: reduces the mortality but increases the intubation risk? Intensive Care Medicine.
- Vanessa Martins de Oliveira et al., 2016. Good practices for prone positioning at the bedside: Construction of a care protocol. Revista da Associação Médica Brasileira
- Section 8: Repositioning and Mobilization. Page 126
- Section 8: Repositioning and Mobilization: Recommendation 5.10. Page 126
- Bellani G et al., 2016. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. The Journal of the American Medical Association.
- Kim RS et al., 2016. Preventing Facial Pressure Ulcers in Acute Respiratory Distress Syndrome (ARDS). Journal of Wound Ostomy & Continence Nursing.
- Richard H Kallet. 2015. A Comprehensive Review of Prone Position in ARDS. Respiratory Care.
- Messerole E et al., 2002. The Pragmatics of Prone Positioning. American Journal of Respiratory and Critical Care Medicine.
- Bamford P et al., 2019. Guidance for Prone Positioning in Adult Critical Care. The Faculty of Intensive Care Medicine & Intensive Care Society.
- Kenney L , Rithalia SVS . 1999. Mattress & bed resource file: assessment of support surfaces. J Wound Care (Suppl); Part 2: 1-8
- Twiste M & Rithalia S.. 2008. Measurement system for the evaluation of alternating pressure redistribution mattresses using pressure relief index and tissue perfusion– a preliminary study. Wound Practice and Research. Volume 16.
- Section 10: Support Surfaces: Recommendation 7.5. Page 163
- Malbrain M, Hendriks B, Wijnands P, Denie D, Jans A, Vanpellicom J, De Keulenaer B. 2010. A pilot randomised controlled trial comparing reactive air and active alternating pressure mattresses in the prevention and treatment of pressure ulcers among medical ICU patients. J Tissue Viability. 19(1), 7-15.
- Section 10: Support Surfaces: Recommendation 7.7. Page 165
- Section 10: Support Surfaces. Page 159
- Robert K. Jensen. 1989. Changes in segment inertia proportions between 4 and 20 years. Journal of Biomechanics.
- Section 9: Heel Pressure Injuries. Page 145
- Clark M, Rowland LB, Wood HA, Crow RA. 1989. Measurement of soft tissue thickness over the sacrum of elderly hospital patients using B-mode ultrasound. J Biomed Eng.
- Abed Elahad, J., McCarthy, M.W., Goverman, J. et al. 2018. An Overview of Sacral Decubitus Ulcer. Curr Trauma Rep.
- Section 10: Support Surfaces: Good Practice Statement 7.9. Page 169
- World Health Organization-Interim guidance. 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected.
- Wonsup Lee et al., 2018. A 3D anthropometric sizing analysis system based on North American CAESAR 3D scan data for design of head wearable products. Computers & Industrial Engineering.
- Section 6: Preventive Skin Care: Recommendation 3.4. Page 88
- Section 2: Etiology. Page 22
- Section 10: Support Surfaces. Page 157
The references listed below by page number, refer to direct statements appearing in the full version of the European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA: 2019.

